Team Members
Julia Carr
Elsa Lindboom
David Nugent
Supervisors
Laurel Carney, PhD, Biomedical Engineering, UR
Customer
Curbell Medical
Description
Patient falls are the largest category of reportable incidents within hospitals. As such, one of the primary motivations for a patient to get up from a seated or reclined position, putting themselves in a situation where a fall is more likely to occur, is the need to toilet (Carroll, Dykes, & Hurley 2010). These falls can result in harm to the patient as well as cost hospitals a considerable amount of money in recovery costs. A 2012 study found the average hospitalization cost following an injury due to a fall to be $34,294 (Falls Cost U.S. Hospitals n.d.). Due to this, there has been a large push in the development of preventative measures that have the potential to reduce the amount of patient falls, specifically in the setting of healthcare facilities. Curbell Medical, a leading medical device manufacturer specializing in the area of signaling devices used in the healthcare field, is one of the companies looking to find a solution to this problem. Working with a 2018/2019 University of Rochester senior design team, Curbell supported the development of a wearable bladder monitoring device that functions through the use of bioimpedance (Alatise, Garcia, Gardiner, & Selmi 2019). This device serves to detect when the bladder is full or close to full and alert health practitioners responsible for the patient that they will likely have to toilet soon. This would give caretakers time to make it to the patient to assist them before they attempt to make it to the bathroom themselves, ultimately preventing a potential fall.
In order to validate and test the efficacy of Curbell Medical’s bladder sensor device, a functional bladder phantom that sits in a model of the human torso must be designed and developed: the project tasked to our design team. This model must be anatomically comparable to that of the average human in terms of structure, electrical properties, and urine filling and voiding functionality.
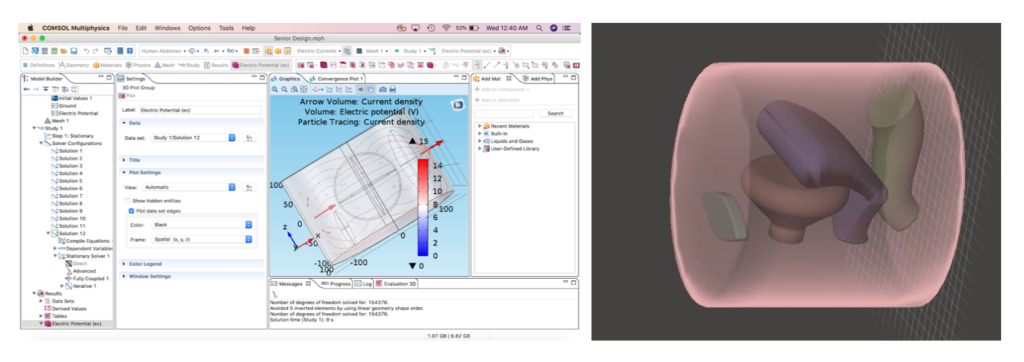
Due to the change in the structure of our coursework following the circumstances surrounding COVID-19, all of our design work is to be completed remotely. This has led our team to adapt the deliverables intended for our customer accordingly, so that the simulation and testing of our intended model can be completed in this remote manner. We have been working to create a model of the human torso in SolidWorks as well as running a FEA model simulation illustrating how the bioimpedance sensor interacts with the body.
While our team is no longer able to complete the fabrication of a physical human abdomen model, we feel that the testing completed to date, both on campus and remotely, as well as the instructions we have laid out for further testing will provide our customer with a helpful framework in order to complete the development of this model.
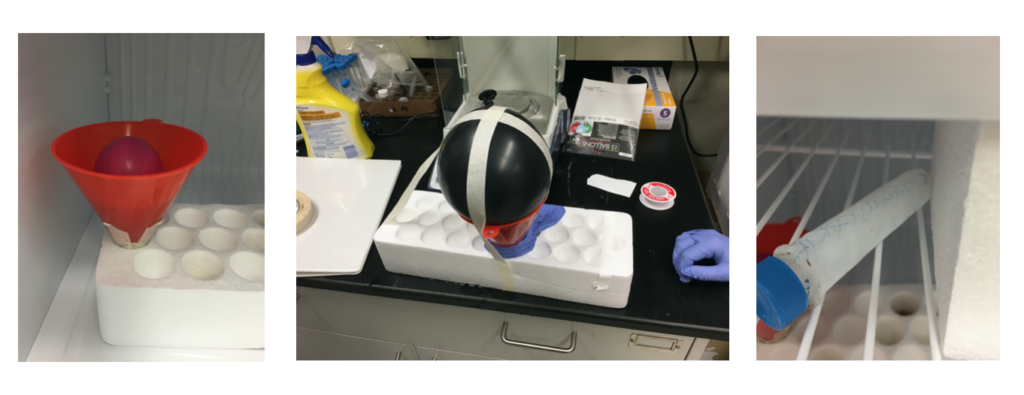
Physical Prototyping
Electronic Computer Modeling
Acknowledgements
Amy Lerner, Ph.D. – Associate Professor of Biomedical Engineering
Art Salo – Biomedical Engineering Laboratory Engineer
Kimberly Richards – Graduate Teaching Assistant
Laurel Carney, Ph.D. – Professor of Biomedical Engineering
Mark Buckley, Ph.D. – Professor of Biomedical Engineering
Moriana Garcia – Biomedical Engineering Reference Librarian
Scott Seidman, Ph.D. – Professor of Biomedical Engineering
Whasil Lee, Ph.D. – Assistant Professor of Biomedical Engineering
University of Rochester Medical Center
Martha Gdowski, Ph.D. – Associate Professor of Neuroscience
Jonathan Stone, M.D. – Assistant Professor of Neurosurgery
Ramzi El-Hassan, M.D. – University of Rochester School of Physical Medicine and Rehabilitation Resident
Curbell Medical
Dan MacDonald – Senior Electrical Design Engineer
Donald Gibson – Vice President of Marketing
Donald Young – Senior Product Manager
George Reamsnyder – Product Specialist
Joel Jusiak – Senior Mechanical Engineer
Thomas Kennedy – Director of Engineering
Thomas O’Connor – Mechanical Engineering Manager
References
Alatise, K, Garcia, C, Gardiner, A & Selmi, A, 2019, ‘Bladder Monitor Device Team Executive Summary’, University of Rochester. [20 October 2019].
Carroll, DL, Dykes, PC & Hurley, AC 2010, Patients’ perspectives of falling while in an acute care hospital and suggestions for prevention. Applied nursing research: ANR. Available from: <https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3107724/>. [20 October 2019].
Falls Cost U.S. Hospitals $34 billion in Direct Medical Costs. n.d., Johns Hopkins HealthCare Solutions. Available from: <https://www.johnshopkinssolutions.com/newsletters/falls-cost-u-s-hospitals-30-billion-in-direct-medical-costs/>. [23 October 2019].
