Problem Statement
Falls experienced in hospitals are common and dangerous. Patients are at an especially high risk of experiencing a fall during trips to the bathroom [1]. Bladder bioimpedance can be used to quantify a patient’s bladder fullness. Monitoring of this information allows a caregiver to help the patient to the restroom without them needing to ask for assistance.
Purpose
Our proposal centers on designing a comfortable and non-intrusive device to measure bladder impedance, determining an individual’s bladder fullness and reducing patient falls. Based on research, the team found that a tetrapolar electrode system could be a viable solution for electrode configurations to ensure the best signal acquired. It suggests that the best placement for electrodes have two placed on the hips (M3 & M4), and two placed next to the navel (S1 & S2) [2, 3, 4].
Design & Overall System
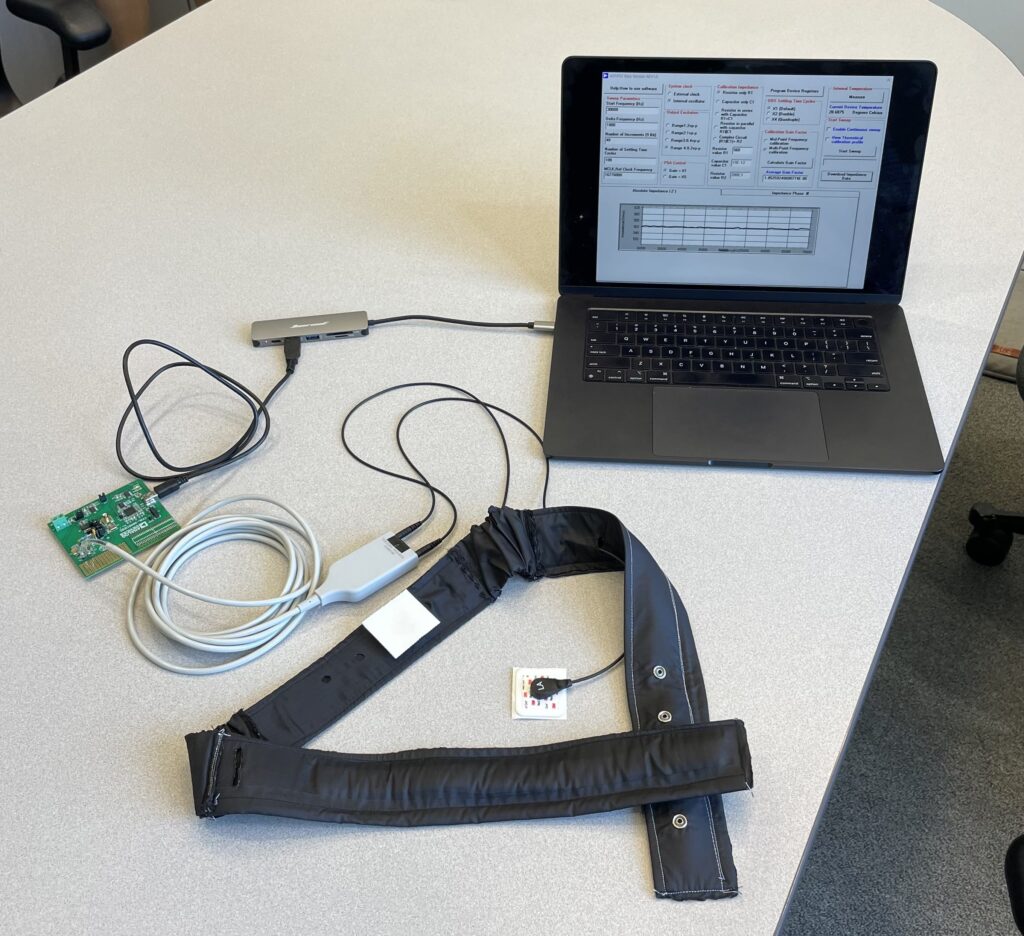
The image below highlights 1) how the device is worn, 2) how the device records the bladder impedance and 3) the belt structure.
Design Considerations
The table emphasizes key components and reasonings behind our design choices. The main focus of our wearable belt is to provide a comfortable interface while also maintaining the ability to adjust for various body sizes.
| Belt Component | Features and Purpose |
| Main Body | Cushioning: Prevent pressure ulcers Seatbelt: Provide structure |
| Nylon Cover | Waterproof Sanitizable Non-irritating |
| Back Fastener | Snap buttons: Flat and comfortable to lay on for extended period of time Multiple snap holes: Provide further adjustability for overall fit |
| Elastic Connectors | Comfortable adjustment between hip and navel electrodes |
| Electrode Leads/Holes | Four electrode holes: Placement of four leads for accurate signal collectionMultiple navel lead holes: Provides flexibility |
Final Prototype
The images below show the final belt design as well as the computer setup to collect data.

Conclusion
Our process suggests that the design of our wearable electrode belt is sound. We were able to demonstrate bioimpedance trends similar to those described in the literature. With future investigation and improvements, our device could be very beneficial for increasing patient safety and establishing a more proactive approach in fall prevention.
Future Improvements
Our device provides a substantial first step in the development of this product. However, with the following improvements listed below, our device could be more fully functional and wearable in its intended clinical setting.
Condensed Circuitry: Currently, an external bioimpedance processing chip and computer is used to gather our impedance values. This chip and computer ideally would be condensed into a microchip and incorporated into the belt. Additionally, including potential bluetooth capabilities to transfer the signal externally could help monitor patients.
Sizing: Multiple iterations of the belt will be developed at various sizes to accommodate all patients.
Alarm System: Using the bioimpedance signal, the next vital step would be to create an alarm system that would notify the provider when a patient needs assistance.
Advanced Calibration: Different people have different bathroom needs based on water intake, electrolytes, diet, or ‘an anxious bladder’ which affect the accuracy of the device. Ideally the device should work for all patients.
Acknowledgements
We would like to thank Dr. Ganeshan, Kaveri Salunke, and Dr. Seidman for their aid in our project. We would also like to thank the personnel at Curbell Medical. Including Donald Gibson, Garrett Mattimore, Thomas Kennedy, Kelly O’Connor and specifically Dan Macdonald, for sending us materials as well as assisting us along the project.
Customer
Led by Donald Gibson, Thomas Kennedy, Dan MacDonald, Garrett Mattimore and Kelly O’Connor.
The Team

Nick Dente, Kate Isaac, Lam Nguyen, Fiorella Rivadeneira, Isabella Smith
Faculty Supervisor: Dr. Veena Ganeshan
Project Management Liasion: Kaveri Salunke
References
1. D. Gibson and T. Kennedy, “Curbell Medical – Wearable electrode system for bladder bioimpedance measurement,” BME 295 Course Materials, Pitch Videos, University of Rochester Blackboard
2. D. Leonhäuser et al., “Evaluation of electrical impedance tomography for determination of urinary bladder volume: comparison with standard ultrasound methods in healthy volunteers,” BioMedical Engineering OnLine, vol. 17, no. 1, Jul. 2018.
3. Y. Yang and J. Wang, “New Tetrapolar Method for Complex Bioimpedance Measurement: Theoretical Analysis and Circuit Realization,” 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, 2005, pp. 6605-6607.
4. H. Yoon et al., “Bladder Volume Measurement With Electrical Impedance Analysis In Spinal Cord-Injured Patients,” American Journal of Physical Medicine & Rehabilitation, vol. 77, no. 6, Nov. 1998.
