Team Members
Joe Criscione
Robert Breidenstein
Jack Donlon
Supervisors
Dr. Danielle Benoit, PhD
Customers
Dr. Ayesha Baig, MD
Description
The aim of this project was to design a device capable of removing impacted food boluses in pediatric patients both more efficiently and more quickly compared to current industry standards.
Background
Studies have found that there are roughly 39,000 cases of impacted food boluses in the U.S. annually, about 90% of which are caused by an underlying pathology (Ho et. al. 2008). The most common pathology seen in the pediatric populations is eosinophilic esophagitis (EoE). This disease presents as chronic inflammation and results in the formation of fibrous strictures that restricts the passage of food through the esophagus (AAAAI, Eosinophilic Esophagitis). Thus, EoE increases the risk of food becoming impacted in the esophagus and not being able to pass into the stomach.
When food becomes impacted it prevents the passage of other substances, leading to pain and irritation. While impacted food boluses are rarely fatal, surgery is still required. The bolus must be removed via endoscopy and the patient must be put under general anesthesia.
The devices currently used to remove impacted food boluses all require that the bolus be broken up and extracted in a piece-wise fashion. This results in a lengthy procedure that may take as long as four or more hours. This is especially troubling for pediatric patients, as the long-term effects of anesthesia on cognitive and emotional development are not well understood.
Problem Statement
The problem our group has been tasked with solving is finding a more effective device to remove impacted food boluses from the esophagus. Our main objective is creating a device which could significantly reduce the length of time the food bolus extraction procedure takes. We intend to do this by creating a device capable of removing larger portions of the bolus in each retrieval attempt.
Design
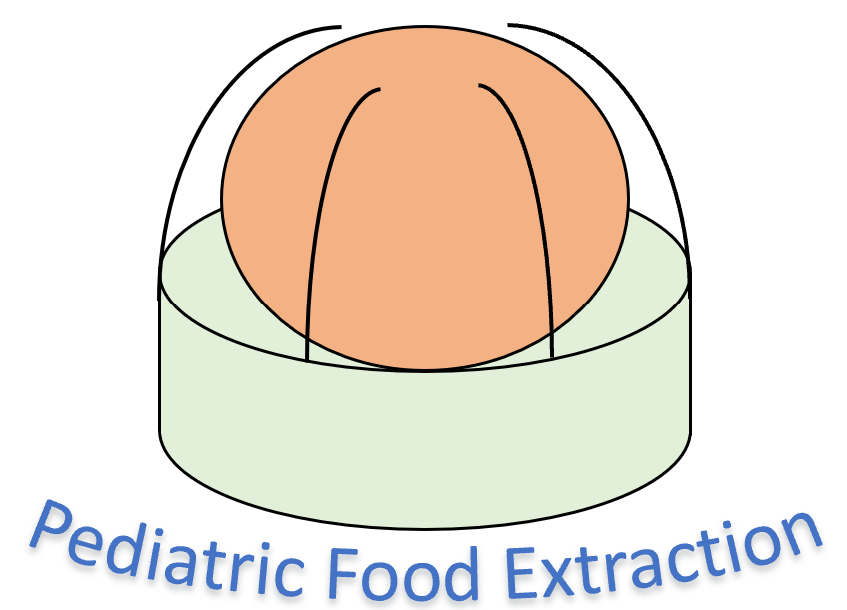
The current design that our group decided on was a hybrid of a suction cap and pronged grasper with the addition of surgical netting. The choice to use a hybrid model was born out of the desire to have suction as the main form of grasping the food bolus, but prongs and netting to retain the initial grasp during extraction. Some key design elements of the apparatus include, the cap shape and design, the prongs shape and design, and the prong-cap integration.
Cap Design:
The suction cap was designed to provide a complete vacuum seal and to assist in the deployment of the prongs. The cap was modeled after the Olympus E-suction endoscope attachment. Like the predicate devices, our suction cap will be made of a flexible elastomer, likely medical grade silicone. Additionally, embedded channels throughout the cap will allow the for the insertion of the prongs.
Prong Design:
The purpose of the prong design is to help aid in the retention of the food bolus. The prong is going to be manufactured out of spring steel to provide rigidity with the ability to bend. The overall shape of the prong is an elispse. An elispse removes the occurrence of sharp corners while maintaing a major and minor axis. The presence of the minor axis naturally causes the prongs to favor bending in a perpendicular fashion. Lastly, a bulbus end will be added to prevent the prong from being pointed and reduce its ability to pierce through the accompanying tissue.
Cap-Prong Integration:
Integration of the prongs and net is achieved through the channels of the cap. Additionally, to increase the ease of insertion of the prongs into the cap, guide channels that extended partially into the main channel of the cap were added.
Use Sceniario
When the food extraction device is used it must first be assembled. Then it can be inserted into the esophagus to extract the food bolus. This process is repeated until the bolus is completely removed or can pass through the stricture on its own.
Assembly:
To assemble our device the prongs are first fed through the auxiliary channel of the endoscope. Once they emerge through the end of the auxiliary port of the endoscope they are individually fed through the guide channels of the sucction cap. Next, the cap is pushed onto the end of the endoscope and sealed via friction. Lastly, the snare is fed through the bulbous ends of the prongs and secured with a surgical knot.
use:
After being properally assembled our device is ready for use. The device as well as the distal end of the endoscope are lubricated with surgical grade lube. Then the endocope is inserted into the patient’s esophagus by the Gasterointerologist through a bite block to prevent damage to the endoscope. Once the food bolus is found, suction is initiated. Through the initial sucction the food bolus is grasped. Next, the prongs are extended to surround a larger portion of the bolus. The snare is then retracted to close the prongs around the food bolus. With both the force of sucction and the prongs pull, the food bolus is removed from the patient. The food bolus piece is then removed from the cap and the process is repeated until the food bolus is completely removed or passes through the stricture on its own.
Acknowledgements
We would like to thank our professors, Dr. Amy Lerner and Dr. Scott Seidman, our customer, Dr. Ayesha Baig, our supervisor, Dr. Danielle Benoit, and our TA liaison, Anna Olsen. Thank you for all of your assistance in making this year a success!
References
“Eosinophilic Esophagitis (EoE).” AAAAI.com, www.aaaai.org/conditions-and-treatments/related-conditions/eosinophilic-esophagitis. International Anesthesia Research Society. journals.lww.com/anesthesia.
Ho, KinKin, and Robert Enns. “Review of food bolus management.”Canadian Journal of Gastroenterology, vol. 22, no. 11, 22 Oct. 2008, pp. 805-08, www.ncbi.nlm.nih.gov/pmc/articles/PMC2661297/. 3
