Cell and Tissue Engineering
What is Cell and Tissue Engineering?
Cell and tissue engineering seeks to understand and control the behavior of cells and tissues, focusing on how environmental factors—such as chemical and physical influences—affect cell growth, differentiation, and behavior. By using innovative materials, cell growth techniques, and genetic modifications, researchers in this field aim to improve medical treatments and outcomes.
Areas of Focus
Our biomedical engineers are leading cutting-edge studies to:
- Develop advanced biomaterials for tissue regeneration and repair across various organs, including bone, cartilage, muscle, skin, and nerve tissues.
- Explore innovative approaches in stem cell therapies for the repair and regeneration of cardiac, hepatic, renal, and pancreatic tissues.
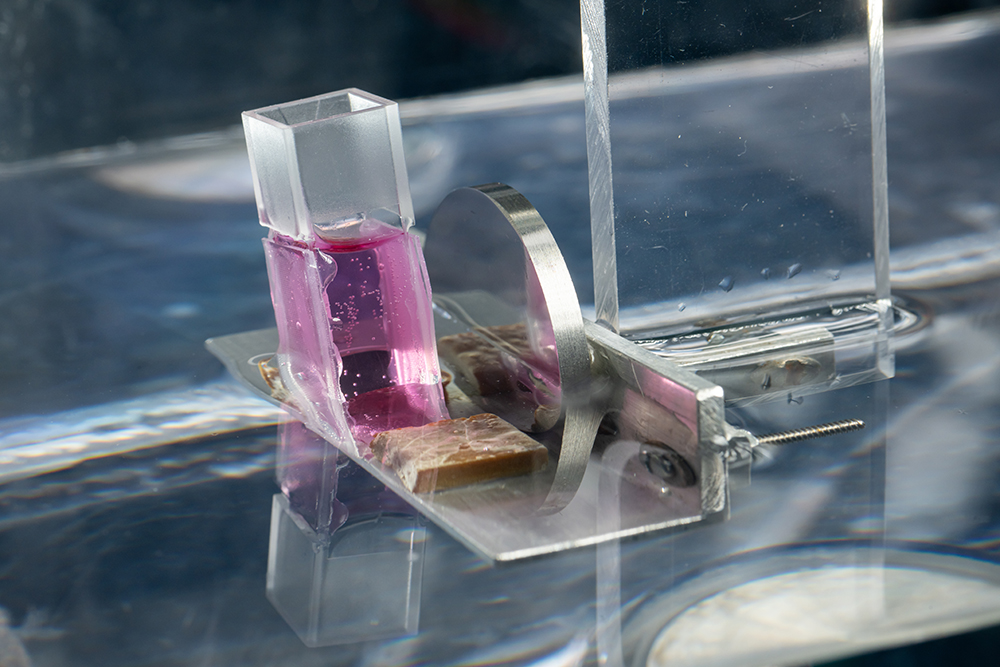
- Use ultrasound technology, microfluidic systems, and other advanced tools for targeted drug delivery, cell culture, and therapeutic applications.
- Investigate the role of extracellular matrices and mechanical forces in influencing cell behavior, growth, and tissue development.
- Design and optimize medical tools, sensors, and systems for personalized, effective healthcare solutions.