Next stop for Falling Walls Competition winner: Berlin
 Kilean Lucas admits to being uneasy about trying to summarize his research in three minutes, with only three slides.
Kilean Lucas admits to being uneasy about trying to summarize his research in three minutes, with only three slides.
You wouldn’t have known it yesterday, when Lucas, a PhD student in biomedical engineering, placed first at the University’s Falling Walls competition.
Lucas won $500 and an all-expenses paid trip to represent the University at the international Falling Walls competition in Berlin this fall.
Lucas described how the silicon nanomembranes developed in the lab of his advisor, James McGrath, could be used to filter out telltale exosomes (small, cell-derived vesicles) from the blood to provide early detection of cancer.
“There’s a lot of weight off my shoulders,” he said afterwards. “I was very nervous about coming to this and being able to communicate my project clearly in three minutes. That’s the hardest part of this.”
So how did he prepare?
With a big assist from his mentor and colleagues.
“I came up with the slides with help of professor McGrath,” Lucas said. Then I came up with a script that I tried out on my lab mates.”
Their feedback helped Lucas through four revisions of the script.
”Then I got together a group of people including my advisor and random people around the department and did a dry run. They gave me a lot of feedback,” Lucas said. In fact, he added, laughing, “ They tore my script apart. I completely reworked it yesterday.”
Sixteen competitors presented in front of a faculty panel that included jury chairman Richard Waugh, interim dean of faculty and associate vice president for research; Kim Arcoleo, associate dean for research at the School of Nursing; Dirk Bohmann, senior associate dean for basic research at the School of Medicine and Dentistry (SMD); Stephen Dewhurst, vice dean for research at SMD; Wendi Heinzelman, dean of the Hajim School of Engineering and Applied Sciences, and Joan Saab, chair of art and art history.
Runner up Kevin Mazurek, a post doctoral fellow in neurology, described a neurorehabilitative approach to help victims of stroke or other brain injury regain the ability to perform daily tasks.
Neurosurgery resident Jonathan Stone, the third place winner, described how patient-specific models of simulated tissue could help surgeons practice difficult procedures ahead of time.
The Falling Walls competition commemorates the fall of the Berlin Wall by giving young entrepreneurs and inventors from around the world the opportunity to express ideas about how to “break down the walls” hindering progress in dealing with challenges confronting science and society.
Lucas’ three-minute presentation:

Today I am going to talk to you about breaking the wall of cancer diagnostics.
Over the course of our lifetime, we have a 40 percent chance of developing cancer, and a 20 percent chance of dying of cancer. Late stage cancers present the highest risk of death as they are like a hydra.
Removing one tumor, or one head, does not guarantee that we kill the whole beast. In fact early diagnosis of cancer can save the lives of over 4 million people around the world each year.
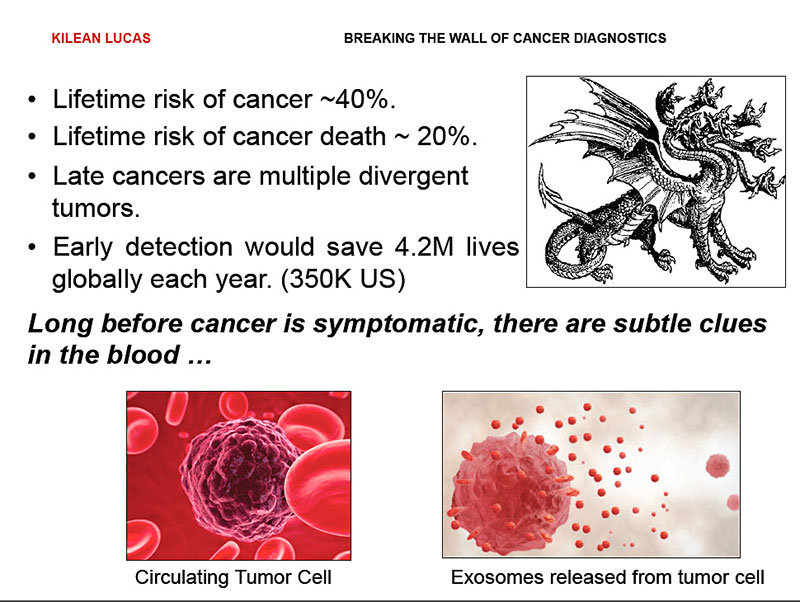
Conveniently, long before cancer presents outward symptoms, it releases subtle clues into the bloodstream in the form of circulating tumor cells and exosomes –50 nanometer vesicles that are basically breadcrumbs of information,
These exosomes contain micro RNA and proteins that are unique to the cells of origin, and provide us with a fingerprint of all the cells present in our body.
While they have all the information we need for diagnosis, searching for them is like searching for needle in haystack. Blood is a multicomponent system, and this makes it very difficult to easily search for these breadcrumbs.
However, what’s the best what to look for a needle in a haystack?
We need to filter out the hay.
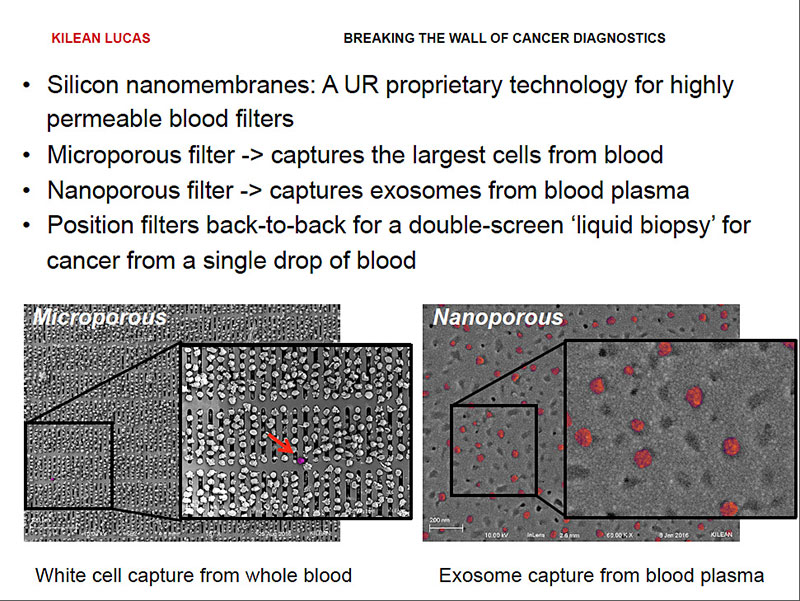
For blood, we have developed exactly the filters we need to do this.
Silicon nanomembranes are one-of-a kind-technology that has been developed right here at the University of Rochester. We have the ability to uniquely tune their pores for highly specific size cutoffs.
This allows us to take membranes with pores that are micrometers in size to completely remove all the cells from blood, including circulating tumor cells, leaving us with only the exosome containing plasma. We can then take that plasma and pass it over second membrane with nanometer sized pores, filtering out remaining proteins and capturing the exosomes.
By pairing these membranes back to back, we can incorporate them in a single device that we can put in front of a routine blood test, giving us an unobtrusive liquid biopsy for breaking the walls of early cancer diagnostics.
